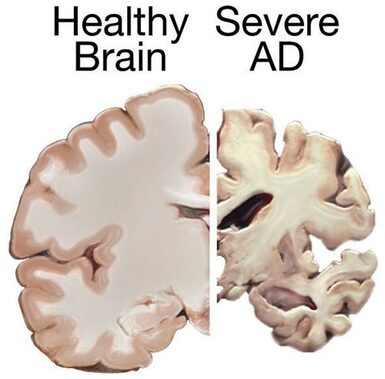
 In this blog I have pointed out that there is a progression in emerging fields of scientific inquiry where competing theories are evaluated, those that do not fit the evidence fall out of favor, and scientists coalesce around a unifying theory that better explains the phenomena they are studying. However, even as a new theory that better fits the available data is accepted in the field, there are individuals who contest the newfound wisdom. Instead of accepting the prevailing thinking, these individuals buck the trend, think outside the box, and propose new ways of interpreting the data. I have referred generically to individuals belonging to this group of scientists that “swim against the current” as “The Unreasonable Men”, after George Bernard Shaw’s famous quote, and I have stated that science must be defended from them. The reason is that science is a very conservative enterprise that gives preeminence to what is established. Science can’t move forward efficiently if time and resources are constantly diluted pursuing a multiplicity of seemingly farfetched ideas. However, this is not to say that the unreasonable man should not be heard. There are exceptional individuals out there who have revolutionary ideas that can greatly benefit science, but there is a time for them to be heard. One such time is when the current theory fails to live up to expectations. I am writing this post because such a time may have come to the field of science that studies Alzheimer’s disease (AD). Alzheimer’s disease is a devastating dementia that currently afflicts 6 million Americans. The disease mostly afflicts older people, but as life expectancy keeps increasing, the number of people afflicted with AD is projected to rise to 14 million by 2050. The disease is characterized by the accumulation of certain structures in the brain. Chief among these structures are the amyloid plaques, which are made up of a protein called “beta-amyloid”. The current theory of AD pathology holds that it is primarily the accumulation of these plaques, or more specifically their precursors, which is responsible for the pathology. Therefore, it follows that a decrease in the number of plaques should be able to alleviate or slow down the disease. This has been the paradigm that pharmaceutical companies have pursued for the past few decades in their quest to treat AD. Unfortunately, this approach hasn’t worked. For the past 15 years or so, every single therapy aimed at reducing the amount of beta-amyloid in the brain has led to largely negative results. In fact, some patients whose brains had been cleared of the amyloid deposits nevertheless went on to die from the disease. Several arguments have been put forward to explain these failures. One of them is the heterogeneity in the patient population. Individuals that have AD often have other ailments that may mask positive effects of a drug. According to this argument, performing a trial with patients that have been carefully selected stands a greater chance of yielding positive results. Another argument is the notion that many past drug failures have occurred because the patient population on which they were tested was made up of individuals with advanced disease. According to this argument, drugs will work better with early-stage AD patients that have not yet accumulated a lot of damage to their brains. Even though many researchers still have hopes that modifications to clinical trials like those suggested above will have the desired effect as predicted by the amyloid theory, an increasing number of investigators are considering the possibility that this theory is more incomplete that they had anticipated and are willing to listen to new ideas and open their minds to the unreasonable man.  One example of these men is Robert Moir. For several years he has been promoting a very interesting but unorthodox theory of AD and getting a lot of flak for it. He dubs his hypothesis “The antimicrobial protection hypothesis of Alzheimer’s disease”. According to Dr. Moir, the infection of the brain by a pathogen or other pathological events triggers a dysregulated, prolonged, and sustained inflammatory response that is the main damage-causing mechanism in AD. In this hypothesis, the production and accumulation of the amyloid protein by the brain is actually a defense mechanism! Dr. Moir agrees that sustained activation of the defense response will lead to excessive accumulation of the amyloid protein and that this eventually will also have detrimental effects. However, even though reduction in amyloid protein levels may be beneficial, accumulation of the amyloid protein is but one of several pathological mechanisms. Moir stresses that the main pathological mechanism that has to be addressed by AD therapies is a sustained immune response, which over time causes brain inflammation and damage. He considers that accumulation of the amyloid protein is a downstream event, and it is known that the brain of people with AD exhibits signs of damage years before any amyloid accumulation can be detected. But much in the same way that Dr. Moir has been promoting his unconventional theory, there are many other theories proposed by others. Oxidative stress, bioenergetic defects, cerebrovascular dysfunction, insulin resistance, non-pathogen mediated inflammation, toxic substances, and even poor nutrition have been proposed as causative factors of AD. This is the big challenge that scientists face when opening their minds to the arguments of the unreasonable man: there is normally not one but many of them! So who is right? Which is the correct theory? And why should just one theory be right? Maybe there is a combination of factors that in different dosages produce not one disease but a mosaic of different flavors of the disease. And maybe the amyloid theory is not totally wrong, but just merely incomplete, and it needs to be expanded and refocused. Or maybe the beta-amyloid theory is indeed right and all that is required for success is to tweak the trial design and the patient population. Maybe, maybe, maybe… When a scientific field is beginning, or when it looks like a major theory in a given field is in need of reevaluation, there always is confusion and uncertainty. Scientists in the end will pick the explanation(s) that better fits the data and take it from there. They did that when most scientists accepted the amyloid theory and they will do it again if this theory is found wanting. The new theory that replaces the amyloid theory will not only have to explain what said theory explained, but it will also have to explain why the old theory failed and what new approach must be followed to successfully treat the disease. In the meantime, Dr. Moir’s theory, along with a few others, is the center of focus of new research evaluating alternative theories to explain what causes AD. The amyloid theory or aspects of it may still be salvageable, but in the field of AD it certainly looks like the time for the unreasonable man has come. Note: after I posted this, I became aware of an article published in the journal Science Advances that proposes a link between Alzheimer's Disease and gingivitis (an inflammation of the gums). The unreasonable men are restless out there! The image is a screen capture from a presentation by Robert Moir on the Cure Alzheimer’s Fund YouTube channel, and is used here under the legal doctrine of Fair Use.The brain image from the NIH MedlinePlus publication is in the public domain.
0 Comments
|
Details
Categories
All
Archives
June 2024
|
 RSS Feed
RSS Feed